How can I take part in a clinical trial?
Discover what it means to take part in a clinical trial and why it’s so important
Finding a trial
There are various ways to learn about a trial you may be interested in taking part in:
- Your doctor may tell you about a trial that they think might be suitable for you
- You may do your own research. You could start by exploring the Biogen trial finder. There are also online databases, such as clinicaltrials.gov, where you can search for trials relating to your condition that are being conducted across many research sponsors
- You could ask a patient advocacy group. You may be able to find a support group for other people with your condition online. These groups are highly educated about clinical research and will generally be aware of relevant trials that are currently recruiting, and will be happy to help
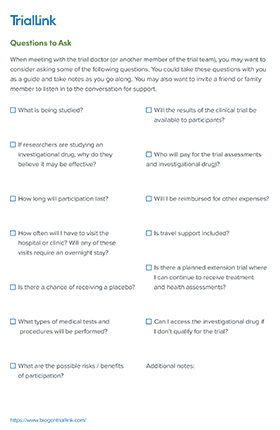
How do I know if I’m eligible to take part in a clinical trial?
A clinical trial is designed for a specific group of people and there are strict guidelines about who can and cannot participate. These are called eligibility criteria.
There are two kinds of eligibility criteria in trials:

Inclusion criteria
Factors that would allow an individual to participate in the trial, such as their age
Exclusion criteria
Factors that would prevent an individual from participating. For example, generally speaking, women who are pregnant, or planning to become pregnant, cannot take part in a trial, in case the investigational drug could have an effect on their unborn baby
Eligibility criteria help researchers identify individuals who can participate in a trial without unnecessary risks.
Don't worry if you’re unsure about whether you’re eligible or not. The trial team will thoroughly check everything they need to know about you against the eligibility criteria before they confirm if you can take part.
And, if they decide you’re eligible, the final decision still rests with you as to whether or not you want to take part.
Is it safe to take part in a clinical trial?
The safety of the people who take part is the top priority of every clinical trial. There are rules and regulations in place to protect both the health and data of everyone who takes part. And if new information regarding safety becomes available after you have decided to join a trial, the investigator will make you aware of it, so you can decide if you wish to continue to take part.
See also Institutional Review Boards and Ethics Committees.
Protecting your rights
There are internationally recognized ethical and scientific quality standards for the design, conduct, recording and reporting of clinical trials that involve humans. For example, Good Clinical Practice (GCP) ensures that the rights, safety and wellbeing of trial participants are protected, and that the results of the trials are credible and accurate. In addition, the Declaration of Helsinki is a statement of ethical principles developed by the World Medical Association to guide physicians and others involved in medical research in humans.
There are also government regulators, such as the Food and Drug Administration (FDA) in the United States and the European Medicines Agency (EMA) in Europe. Every trial has to be approved by national and/or regional regulatory authorities before it can begin.
Protecting your data
Health information, personal data, and identifiable information are protected, confidential and secure, and not shared with third parties. Trial data and samples would only be shared for the purposes of further research if you gave your permission. Only the trial team, people hired to perform or manage the trial, will see personally identifiable data. And only trial data that is de-identified will be shared with the company conducting the trial. ‘De-identified’ means that it cannot be linked back to you. Immigration status is generally not collected in clinical trials and will not be collected in any Biogen clinical trial.
Where next?
If you’re ready to find a trial that may be right for you, try using our trial finder.
Find more information about specific medical conditions that we are researching.